Prostate Cancer – A Simple Guide
If you’ve heard the term “prostate cancer” and felt a bit lost, you’re not alone. It’s a common condition for men over 50, but knowing the facts can make the whole thing feel a lot less scary. In this guide we’ll break down the basics, point out the signs to watch for, and show you what the treatment world looks like today.
First off, the prostate is a small gland that sits just under the bladder. Its main job is to make fluid for semen. Cancer starts when cells in the gland grow out of control. Most cases grow slowly, which is why early detection matters – catching it early often means easier treatment and better outcomes.
Age is the biggest risk factor. Men in their 60s and 70s face the highest chance of developing prostate cancer, and the risk keeps climbing after that. Family history matters too; if a dad or brother had the disease, your odds are higher. Lifestyle choices like a diet high in red meat and low in vegetables might raise risk, while staying active can help keep it down.
Screening is the key to finding prostate cancer before it causes problems. Most doctors recommend a PSA (prostate‑specific antigen) blood test starting at age 50, or earlier if you have a family history. The test isn’t perfect – sometimes it flags harmless bumps – but it gives a useful picture of what’s going on inside.
Common Signs and When to Get Checked
Early prostate cancer often has no symptoms at all, which is why regular screening matters. When signs do appear, they’re usually subtle. You might notice a weak or interrupted urine flow, the need to get up at night to pee, or a feeling that you can’t empty your bladder completely.
Blood in the urine or semen, or pain during ejaculation, can also point to a problem, but they’re less common. If you experience any of these, don’t wait – talk to a doctor. Even a quick check-in can rule out serious issues or catch something early enough for simple treatment.
The PSA test measures a protein that the prostate releases into the blood. Higher levels can mean cancer, an infection, or simply an enlarged prostate. If your PSA is elevated, the doctor may suggest a repeat test, a more detailed blood panel, or a biopsy to get a clear answer.
Another tool is the digital rectal exam (DRE). Your doctor inserts a gloved finger into the rectum to feel the prostate’s surface. It’s quick, a little uncomfortable, but can spot lumps that blood tests miss. Combining PSA and DRE gives a stronger sense of what’s happening.
Treatment Options and Living Well
When cancer is confirmed, treatment plans can vary widely. Your doctor will look at the tumor’s grade, stage, and your overall health. Many men with low‑grade, slow‑growing tumors choose “active surveillance” – monitoring the cancer with regular PSA checks and scans instead of immediate treatment.
If you need to act, surgery is one route. A radical prostatectomy removes the whole gland and some surrounding tissue. Modern techniques, like robotic‑assisted surgery, often mean less bleeding and quicker recovery, though there’s still a risk of urinary or sexual side effects.
Radiation therapy offers another non‑surgical path. External beam radiation targets the prostate from outside the body, while brachytherapy places tiny radioactive seeds inside the gland. Both can be effective, and side‑effects tend to be milder than surgery for many patients.
Hormone therapy, also called androgen deprivation therapy (ADT), lowers the male hormones that fuel cancer growth. It’s usually paired with radiation or used when the cancer has spread. ADT can cause hot flashes, fatigue, and bone density loss, so doctors often add bone‑strengthening meds and lifestyle advice.
Beyond medical treatment, lifestyle tweaks help you stay strong. Exercise – especially weight‑bearing and cardio – improves energy and can keep side‑effects in check. A diet rich in fruits, vegetables, whole grains, and healthy fats (think fish and nuts) supports overall health. Staying connected with support groups also makes the emotional side of the journey easier.
Follow‑up care is crucial. Even after treatment, regular PSA tests and doctor visits keep an eye on any recurrence. Most men return to normal activities within a few months, but listening to your body and reporting new symptoms early makes the difference.
Prostate cancer is a big topic, but breaking it down into simple steps – screening, spotting signs, and knowing your treatment choices – puts you in control. Keep the conversation open with your doctor, stay active, and remember that early detection gives you the best shot at a smooth road ahead.
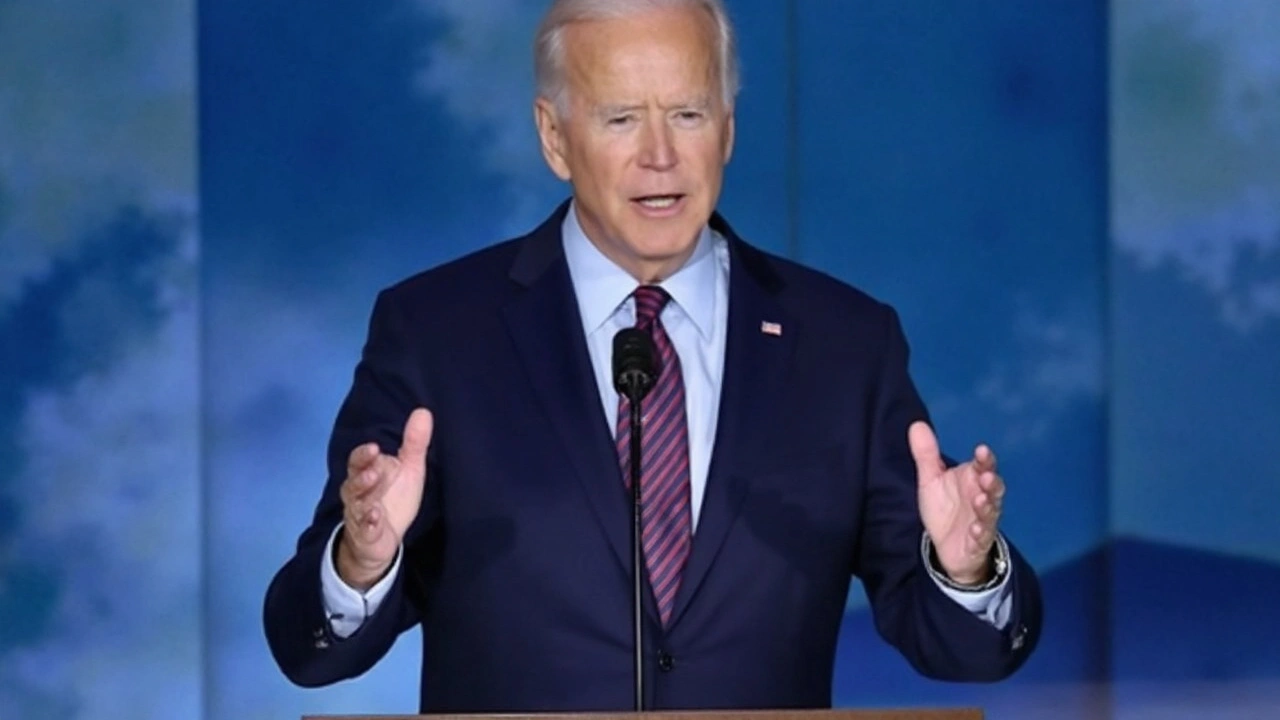
Joe Biden’s Stage 4 Prostate Cancer: What His Diagnosis Means and How Treatment Works
Joe Biden, 82, has been diagnosed with aggressive stage 4 prostate cancer that has spread to his bones. While not considered curable, doctors say patients often live multiple years with current treatments. Biden is reviewing hormone therapy and other options as his case draws national attention to prostate cancer challenges.